
By dietetic intern Blair Strickland and Orli Rabin of ThrivingBiome
First of all, let’s set the record straight on the basics of HRT. Simply put, hormone replacement therapy is medicine that delivers exogenous female hormones to the body. In other words, someone who is on HRT is taking in estrogen that the body is not making on its own, usually after menopause. For this reason, HRT is often called MHT, or Menopause Hormone therapy, and it has been safely used since the 1960’s to treat menopause symptoms, including hot flashes, night sweats, or vaginal dryness.
Though it was safe to use and helped millions of women, HRT became one of the most controversial and polarizing medications in mainstream medicine. Beginning in 2002, the U.S. healthcare system rejected this treatment option for twenty-plus years, following the confusing and widely publicized results of a major clinical trial, the Women’s Health Initiative (WHI). Findings indicated that HRT were more harmful than beneficial to female health, generating alarm and fear among users and prescribing doctors. This resulted in women suffering through menopause symptoms without a viable treatment option.
But the panic and resulting widespread rejection of HRT was largely unfounded, for a couple of reasons. First, the female population in the WHI study consisted of women mostly in their sixties, which is several years older than average menopause onset, when HRT would be most useful for symptom relief. Risk factors were higher for this older population than they would be for the typical user (we’ll talk more about risk factors later). Second, the WHI spread the message that all HRT was dangerous, but it left out important details regarding type and route of administration. Looking back at the study through today’s lens, we also see that participants took a combination of equine estrogen and synthetic progestin – not the safe and widely available forms prescribed today.
While HRT was misunderstood for many years, follow-up studies in the US and Europe demonstrated the beneficial effects of these treatments, particularly when prescribed for symptomatic women within 10 years of the onset of menopause, or who are under 60 years of age. It has taken time for the medical community and public opinion to catch up and understand that these medications are not dangerous, but we are getting closer. Menopause is receiving the credit it deserves as a major health milestone in women’s lives, with very real and often brutal symptoms worthy of treatment. At the same time, estrogen is being recognized as the powerhouse that it is within the female body, impacting everything from mood to bone health to cognition.
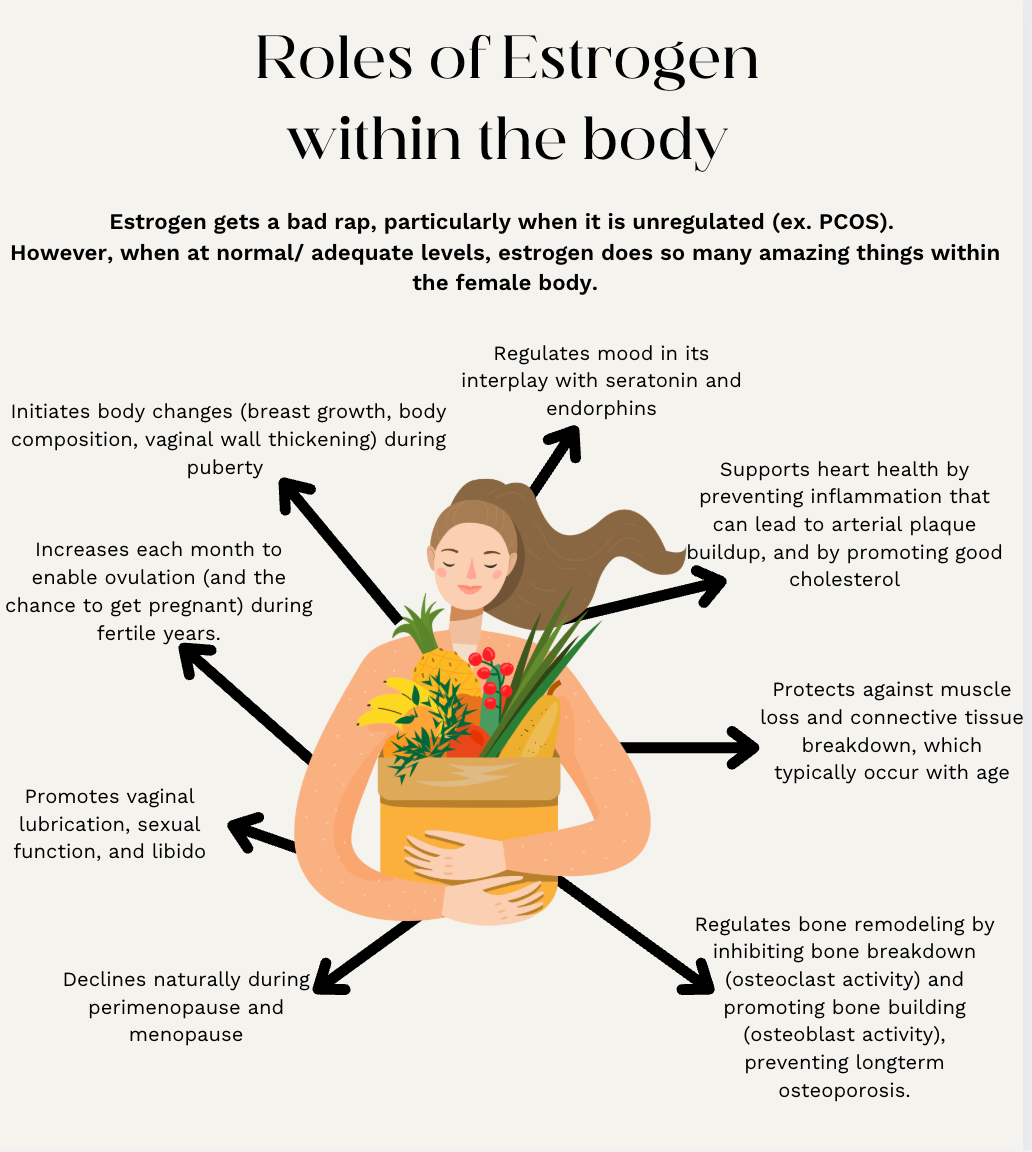
Let’s take a look at estrogen and its role in menopause and perimenopause more closely. Estrogen, along with its counterpart progesterone, are the two critical female sex hormones. Estrogen plays countless important roles in the body, serving as a chemical messenger that initiates and stops processes related to menstruation and sexual health, cardiovascular health, bone health, brain health, and more. In regards to sexual health and function, estrogen levels rise during puberty, enabling the body to make changes (breast growth, body composition, vaginal wall thickening and lubrication) to begin menstruating and allow for reproduction. Each month, estrogen peaks to prepare for ovulation– your “fertile window” – where you could get pregnant if you have intercourse.
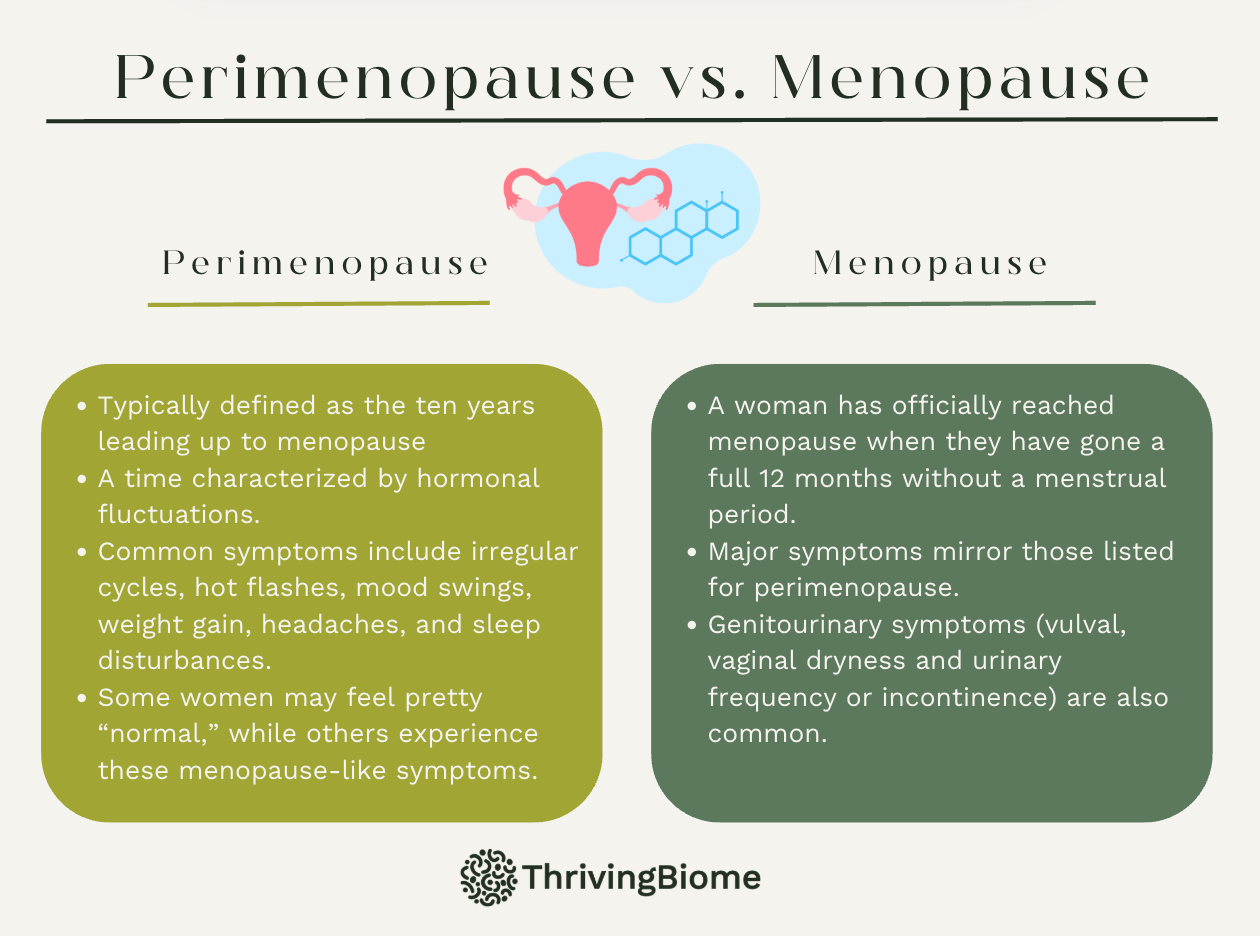
Estrogen levels naturally decline in perimenopause. Usually defined as the ten years leading up to menopause, this is a time of transition, characterized by hormone fluctuations, irregular cycles, hot flashes, mood swings, weight gain, and sleep disturbances. It is a bit of a gray area – some women may feel pretty “normal,” while others experience these symptoms, which mirror the symptoms of menopause.
So, if you are already having these symptoms, what is the difference between perimenopause and menopause? You’ve officially reached menopause when you have gone a full twelve months without a menstrual period. The average age for menopause is around 50, but this can vary person to person. On a hormonal level, your body switches from producing estradiol (E2) to the form of estrogen called estrone (E1).
With this drop in E2, menopause again can present with a cascade of symptoms, which are typically classified as vasomotor symptoms (VMS) – think hot flashes, night sweats, headaches, and genitourinary symptoms (vulval, vaginal dryness and urinary frequency or incontinence). However, there are other issues that can arise around the time of menopause, including higher incidences of cardiovascular disease, and increased osteoporosis and bone fracture risk. These are complex, multifactorial conditions, but it is worth understanding how estrogen is a key player in bone remodeling. Bone is a dynamic organ, being built and broken down all the time. Estrogen regulates this process by inhibiting osteoclast activity (bone breakdown) and promoting osteoblast production (new bone building). Without estrogen onboard, there is more breakdown occurring than rebuilding, and bones become less dense and more fragile, posing a greater risk of fracture.
If you are a premenopausal woman reading this, these symptoms may sound uncomfortable and even scary. We want to pause and acknowledge that menopause is a normal progression of our female physiology, and that not every woman experiences the full spectrum of these symptoms. And there is more good news – HRT is a treatment option that can drastically help.
You may be asking, how is HRT taken, and how does it help? HRT usually consists of some combination of estrogen and progestin. This is important, because estrogen causes thickening of the uterine lining, and progestin helps that lining to shed, lowering risk of endometrial cancer. Two main medication patterns are continuous-combined therapy, in which both estrogen and progestin are both taken daily, and cyclic therapy, in which estrogen is taken continuously and progestin is added in for approximately ten days each month. The most common delivery method is transdermal estrogen patches, followed by estrogen injections and/ or oral pills for those who do not tolerate patches well. Vaginal estrogen is also an option that specifically targets vaginal symptoms. Progestin is normally taken orally in pill form.
With these hormones on board, women may experience noticeable symptom relief, including but not limited to: decreased hot flashes, night sweats, restless sleep, vaginal dryness, brain fog, irritability, and overactive bladder. Less noticeable but equally important long-term benefits include protecting your bones – having estrogen onboard enables bone remodeling and can minimize bone resorption, as well as decreasing risk of cardiovascular disease. While this is not a magic cure erasing all signs of menopause, HRT has the potential to drastically enhance one’s quality of life by improving immediate physical and mental symptoms, sexual wellness, and markers of longevity.
As you consider whether HRT is right for you, there are a few other things to consider. First, a couple of side effects to note. Some women experience vaginal spotting or bleeding, which should subside within a few months. Bloating or fluid retention and breast soreness are also common, but temporary. Finally, some women report headaches early on in treatment. These side effects are relatively minimal, but you might be curious about some other risks of the treatment that you’ve heard about, such as risk of cancer or heart attack. As mentioned, discussion of these risks is typically still rooted in Women’s Health Initiative findings, but here’s what we think you should know.
In terms of cancer risk, estrogen-only therapy causes the lining of the uterus to thicken, which increases risk of endometrial cancer. The addition of progestin greatly decreases this risk. Breast cancer risk and HRT is also a hot topic. Women with a history of hormone-sensitive breast cancer should work with their doctors to take an individualized approach to HRT – it may or may not be right for them. Cardiovascular risk is nuanced, too: as revealed in the WHI study, older women (think 60 plus) who are more than ten years past menopause may be at a slightly higher risk of CVD when taking combined HRT. However, for women within 10 years of menopause and under 60 years old, research suggests HRT’s protective effect against cardiovascular disease. Other determinants such as family history and lifestyle factors come into play here as well. A trusted practitioner can help evaluate the holistic picture of your health to determine whether or not you are a good candidate.
Another term you may have heard thrown around is bioidentical hormones. These are synthetic hormones derived from plants that are similar to those produced within our bodies. They include both FDA approved, mainstream hormonal formulas, as well as compounded drugs, which are not regulated by the FDA. Some providers feel that these are a little riskier because they may vary in strength and composition, but others are comfortable prescribing them. In other words, bioidenticals are not good or bad – they are just another option available, based on a patient’s specific needs and the prescribing practitioner’s preference and recommendation.
We hope we’ve provided you with a thorough yet digestible introduction to hormone replacement therapy. Our goal was to dispel fear and unpack the nuances of what these treatments are, so that you are armed with enough knowledge to discuss them with your doctor and decide if they are right for you, either now or in the future. In addition, we hope that you come away from reading feeling heard and acknowledged if you have been suffering with perimenopausal or menopausal symptoms. Women deserve to feel well regardless of life phase, and HRT is a valuable treatment option during this time of transition.